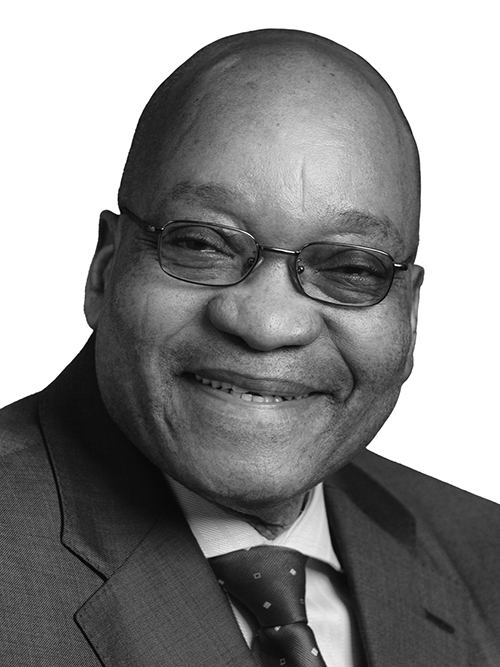
Address by President Zuma at the launch of Operation Phakisa 2: Ideal Clinic Realisation and Maintenance, Sefako Makgatho Presidential Guest House, Pretoria
The Premier of Gauteng, Mr David Makhura,
Ministers and Deputy Ministers,
MECs, Executive Mayors,
Honourable MPs and MPLs,
Directors-General and Senior Government Officials,
Representatives of Labour, the Private Sector, Non-governmental
Organisations, Development Partners and Academic Institutions,
Fellow South Africans,
Good morning.
We are gathered here this morning to witness yet another milestone in our country’s efforts to improve the quality of life of its people, by enhancing their health.
This is the second initiative under our Operation Phakisa programme, which is entitled Ideal Clinic Realisation and Maintenance.
This intervention seeks to transform all our public sector clinics into Ideal Clinics, which provide good quality care to all our communities.
South Africa has a rich and proud history of Community Oriented Primary Care, a frontrunner by many years, of Primary Health Care.
This history dates back to the 1940s, when the late Professor Sydney Kark and his wife Professor Emily Kark established the health centre approach in Pholela, in KwaZulu-Natal, and introduced a community-based approach to health care delivery. The seminal work done in Pholela became a beacon for many countries.
When the apartheid Nationalist government ascended to power in 1948, the pioneering work of the Kark family was reversed. However, their work was not in vain, as Community Oriented Primary Care remains highly relevant to health care delivery in South Africa today.
In 1997, the democratic government of South Africa adopted the White Paper for the Transformation of the Health System, which had its underpinning in this powerful and equalizing philosophy of Primary Health Care.
Over the 20 years of democracy, our country has made major strides towards creating a unified health system rooted in Primary Health Care principles. The White Paper on the Transformation of the Health System of 1997 laid a solid foundation for this.
Our National Health Act of 2004 provides a framework for public accountability through community involvement in health issues.
In addition to a clear outline of the different roles and responsibilities of the different levels of the health system, the legislation provides for the establishment of Clinic Committees, Hospitals Boards and District Health Councils.
Access to Primary Care services, measured in terms of visits to our health facilities, has almost doubled, from just over 67 million headcounts in 1998 to over 130 million headcounts in 2013.
However, we cannot rest on our laurels. South Africa remains an unequal society because of the apartheid history of exclusion and marginalization of the black majority.
The inequality translates into inequality in health care services as well, with rural areas and former homelands being more deprived.
The National Development Plan that we are implementing through programmes such as Operation Phakisa, provides the vision of an ideal health care system.
The NDP talks about “A health system that works for everyone, produces positive health outcomes, and is not out of reach”.
This goal will only be achieved through a well-functioning health system, anchored on Primary Health Care principles.
This philosophy therefore continues to influence and guide our country as we prepare for the realization of universal health coverage for all the people of South Africa, through the implementation of National Health Insurance (NHI).
The Ideal Clinic Realisation and Maintenance Programme is rooted in the ethos of Primary Health Care.
It is not only about further enhancing access to good quality care in our clinics, but is also about fostering closer relations between our clinics and the communities they serve.
It also aims to foster relations between government and non-governmental actors and formations active in those communities.
The question we are to ponder today is the following:
If we were to ask the people of South Africa, ordinary citizens, to define an Ideal Clinic, what would they say?
I am convinced that the masses of our country would define an Ideal Clinic as a health facility that possesses the following characteristics:
It will be a clinic that opens on time in the morning, according to its set operating hours, and which does not close until the last patient has been assisted, even if this is beyond the normal closing hours.
It is staffed by health care providers who treat people with dignity, and observe the Batho Pele principles of Access, Consultation, Courtesy, Information, Service Standards, Openness and Transparency, Redress and Value for Money.
The ideal clinic will provide community-based health promotion and disease prevention programmes in collaboration with the community.
It is very clean, promotes hygiene and takes all precautionary measures to prevent the spread of diseases.
It has reasonable waiting times and community members do not have to sacrifice their entire working day to seek health care.
It provides a comprehensive package of good quality health services every day and community members do not have to return on different days for different services.
It has the basic necessities available, such as essential medicines.
It refers people to higher levels of care timeously when this is required.
It works together with the community it serves, with diverse stakeholders, in promoting health and socio-economic development.
Finally, community members would say an Ideal Clinic is one that we can be proud of, and call it “our own clinic”, rather than a “government clinic” or a “state health facility”.
Does such a clinic exist in South Africa today?
Over the last five weeks, a team of 164 senior managers from the national, provincial and local government spheres of government, together with their counterparts from the private sector, organized labour, academia, civil society and our Public Entities, participated in this Operation Phakisa laboratory to devise ways and means of making the Ideal Clinic concept a reality.
They were supported in this process by officials from the Performance Management and Development Unit in Malaysia, where we learned this big fast results delivery model.
The work of Operation Phakisa: Ideal Clinic Initiative was organized into 8 workstreams focusing on the different building blocks of an ideal clinic capable of delivering good quality health services.
These were the following:
1. Service Delivery
2. Waiting Times
3. Human Resources
4. Infrastructure
5. Financial Management
6. Supply Chain Management
7. Scaling up and Sustainability
8. Institutional Arrangements
The Service Delivery Workstream has developed creative initiatives to ensure that all facilities deliver integrated, comprehensive, and truly holistic health services of optimum quality to ensure satisfactory patient experience and positive health outcomes.
The Waiting Times Workstream has worked hard to produce detailed plans to ensure that 80% of patients will have a positive experience of care, and that 90% of patients will be satisfied with their waiting time, and that no patient will spend more than 3 hours at the clinic, or more than 2 hours waiting for services.
The Infrastructure Team has developed measures to ensure that by 2017, most of our public sector primary care facilities will have world class infrastructure, which will result from quality construction, delivered on time, having been quality assured.
These facilities will also be consistently maintained.
Health care delivery is a labour intensive industry. The Human Resources for Health Workstream has looked at developing measures to ensure that the necessary staff with the right skills is in place to properly deliver the service package in every primary care facility.
Such services must also be provided in a caring and empathetic manner, which is the basic tenet of health care provision.
From the Financial Management Workstream, innovative proposals have emerged for promoting equitable allocation of resources between districts and for improving accountability for public resources. This includes enforcing adherence to allocated budgets and minimizing fruitless expenditure.
The Supply Chain Management Workstream is informed by the fact that public sector clinics regularly run out of supplies.
This team has proposed measures to achieve complete and reliable availability of medical supplies and standard stock items in all clinics and to reduce the costs of procurement and distribution by at least 10%, while lowering the administrative work burden at clinic level, and speeding up the turn-around of non-standard stock items.
The 8th and final Workstream, which looked at Institutional Arrangements, looked at coordination between the three spheres of government, bearing in mind that there are also municipalities that provide primary health care services.
The 8 Workstreams of Operation Phakisa will spend the rest of this week finalising their detailed delivery plans.
A massive change management process is required to roll-out a programme of the magnitude of the Ideal Clinic initiative.
The Scale up and Sustainability Workstream has therefore developed a scale-up framework and an implementation plan for all primary care facilities to achieve sustainable Ideal Clinic status by 2018/2019.
The public will be informed of the outcomes once the process has been concluded.
I will now reiterate what I said in Durban on the 19th July 2014, when we launched the first component of Operation Phakisa focusing on Unlocking the Economic Potential of South Africa’s Oceans.
I will take a personal interest in monitoring progress with the implementation of this Operation Phakisa on Ideal Clinics.
I will receive regular progress reports from Minister Motsoaledi and other Ministers involved in this initiative, with a view to dealing with any challenges that may arise during implementation.
Compatriots,
This week our country has gone through a painful period as we received the mortal remains of our people who died in Nigeria.
We would like to thank and congratulate the Inter-Ministerial Committee that managed the repatriation, under the leadership of Minister Radebe, and all officials who worked tirelessly to make this difficult process a success.
We extend our heartfelt condolences to the family of Mr Peter Furhi, the director of emergency medical services and disaster medicine at the Department of Health who sadly died after contracting malaria in Nigeria.
It is a painful loss for the family and the country as a whole, of an official who was dedicated to serving his people and his country. May his soul rest in peace.
The provincial governments will continue to provide support to the families of the Nigerian tragedy victims until all have been laid to rest.
Ladies and gentlemen, it gives me pleasure to officially launch Operation Phakisa: Ideal Clinic Realisation and Maintenance.
I urge all key role players to support the programme so that we can create the clinics that our people will look forward to visiting for their health care needs.
I Thank you.




